Biomedical Engineering or Normal Nutrition? (SS/Medicaid/Medicare)
The Stoa league debate topic and institutional bias for surgery
Biases (or preferences) are baked into institutions such as the National Institutes for Health. NIH fiscal year 2021 funding of $25 billion is allocated to a variety of research and development projects, including the National Institute of Biomedical Imaging and Bioengineering (NIBIB). (Plus NIH received an additional $5 billion in “Coronavirus Supplemental Appropriations” for FY2020-2021.)
For the current Stoa debate league Lincoln Douglas topic, students advocate and defend values of “restraint” and “scientific advancement” in biomedical research. (Resolved: In the field of biomedical engineering, restraint ought to be prioritized over scientific advancement.)
One natural restraint on advancing biomedical engineering is cost. Resources are limited and the opportunity cost of funding any biomedical research is best measured by the next best alternative uses of that money and time. Government, foundation, or private funding of biomedical engineering has costs that can be measured in what those research funds could accomplish in other medical fields or elsewhere in the economy (or simply saved). Who should decide, and how?
Virginia Mason Franciscan Health in Seattle has a Center for Weight Management page listing options: Surgical weight loss (“laparoscopic and robotic-assisted surgery”), Endoscopic weight loss (“a thin, flexible tube”), and Medical weight loss (lifestyle coaching and medications).
Endoscopic weight loss is explained: “AspireAssist is an FDA-approved weight loss solution” where “a small tube inserted into your stomach connects to a low-profile button on the surface of your skin, through which some of your stomach contents are emptied after eating…” Also offered: “Gastric balloon is a noninvasive procedure that helps you eat less and feel fuller for longer due to a balloon placed into the stomach endoscopically…”
Not listed on the Center for Weight Management page are less expensive and even less invasive nutritional approaches for weight loss: advice to consume less carbohydrates. Tens or hundreds of millions of dollars were spent developing and testing the above biomedical engineering devices and procedures. Biomedical engineering science was advanced with these and dozens of past and prospective weight loss devices and procedures. But common sense suggests restraint is funding research and development of ever more complex biomedical gadgets for weight loss.
If nutritional advice and coaching can provide as good or better weight loss (and type 2 diabetes remission) than gastric surgeries, tubes, bands, and balloons, why not save the money and deploy the research scientists in other medical care fields?
Current technologies are safer and more effective than those in the past. But are they safer and more effective than dietary changes?
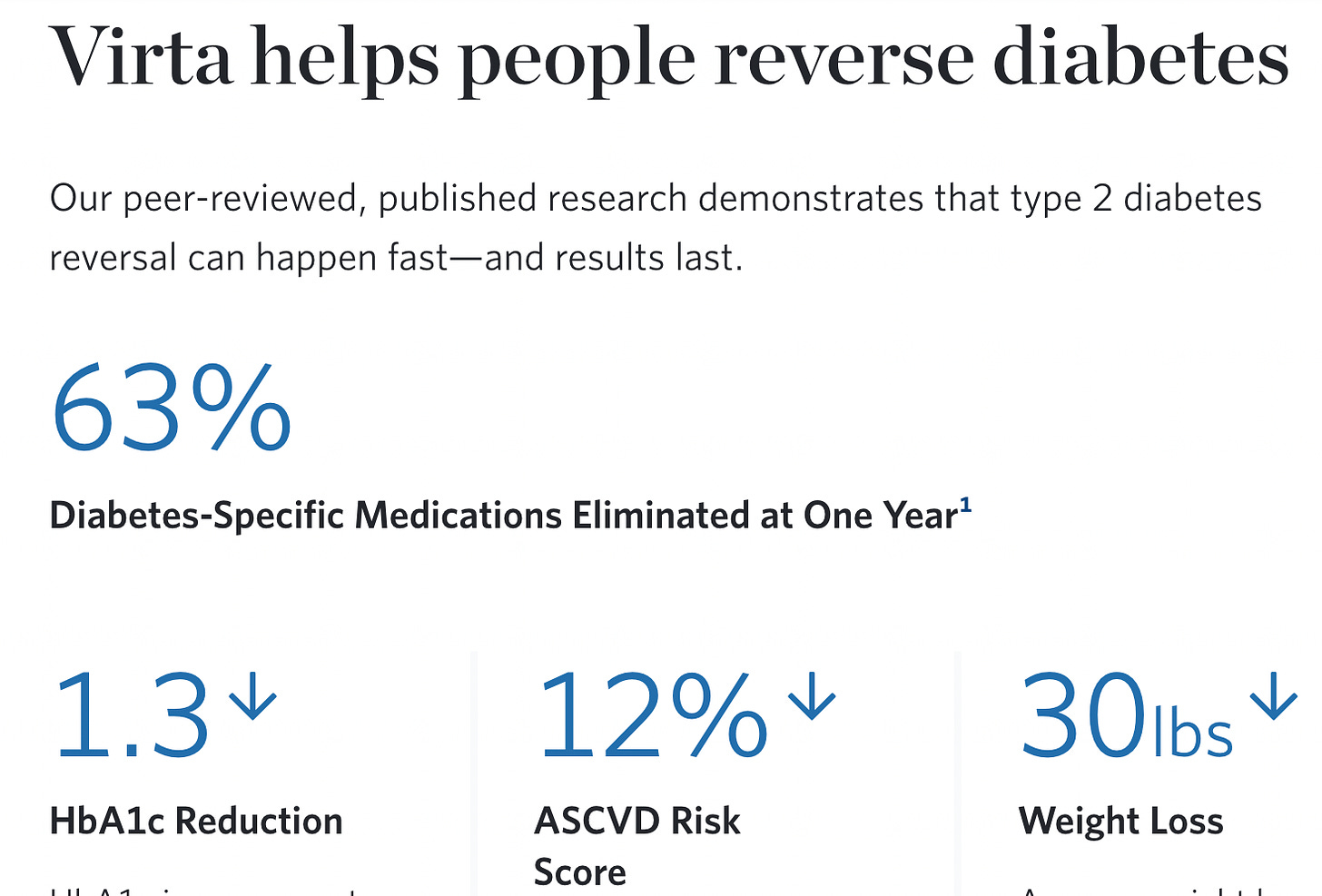
Virta Health advertises: Blood sugar control without the drugs. Our approach helps people lower blood sugar and lose weight, even while eliminating the need for medications, including insulin.
Health Care Economics: Key to SS/Medicaid/Medicare
Fewer people and companies earn income from a weight loss “procedure” that consists mostly in assisting or coaching for dietary changes, namely replacing carbohydrates with healthy fat and protein (perhaps with time-restricted eating). No federally-funded research is needed, though such research would have been helpful to document the lack of research supporting the current high-carb Federal Dietary Guidelines. And in fact no NIH funding of low-carbohydrate research was approved from 1980 to 2012. No wonder there is so little long-term data to show the safety of weight loss from reducing carbohydrate consumption.
The success of nutritional change for addressing chronic health conditions can play a major role in assisting the needed reforms for Social Security, Medicaid, and Medicare programs. The CDC reports 90% of the nation’s $3.8 trillion in annual health care expenditures are for chronic diseases such as obesity, diabetes, heart disease, and mental health conditions. (My Brief Analysis #142 (pdf) and previous Normal Nutrition post discuss the role of federal dietary guidelines causing or contributing to the ongoing obesity/diabetes epidemic.)
Cutting medical costs by 40%, 60%, or more, especially for the elderly who suffer the most from these conditions would allow current funding to cover Medicare and Medicaid costs, as well as allow for Health Savings Accounts to boost retirement savings.
John Goodman’s New Way to Care: Social Protections that Put Families First will be a valuable resource for students if the SS/Medicaid/Medicare topic is chosen.
More information at Cato/Independent event here: New Way to Care: Social Protections That Put Families First:
In his new book, New Way to Care: Social Protections That Put Families First, author John Goodman argues that our most important social insurance institutions are in desperate need of reform. Goodman proposes a simple idea. People of any age should have the choice to opt out of social insurance in favor of alternatives that better meet their individual and family needs. In particular, people should be able to substitute the assets and arrangements they own for the insurance systems that the government currently forces people to participate in.